What is hypoglycemia?
An in-depth guide.
December 10, 2021

Diabetes is characterized by high blood sugar — so you might be surprised to learn that hypoglycemia, or low blood sugar, is common in people with diabetes. Often, these individuals must take insulin to keep their blood sugar in check because their bodies either don’t produce enough of it or don’t respond correctly to this natural check and balance system. But this very same substance designed to maintain blood sugar can often drive blood sugar levels too low, which can result in serious consequences including seizures or coma. Symptoms of hypoglycemia aren’t always obvious, so it is critical for people with diabetes and their caregivers to understand the condition and work to prevent extreme cases.
Low for you may not be low for me
Generally, hypoglycemia occurs when blood sugar (a.k.a. blood glucose) drops below a healthy level. A general rule of thumb for low blood sugar in diabetic individuals is a reading lower than 70 milligrams of glucose/deciliter of blood (mg/dL). However, this is just a rough guideline. Each person has a blood glucose level that is healthy for them and is determined by their doctor. Monitoring this level regularly, whether through a blood glucose meter a few times a day or with a continuous glucose monitor (CGM), can help patients catch hypoglycemia events before they get too serious.
Who is at risk for hypoglycemia?
Hypoglycemia isn’t common in diabetic patients that do not take insulin — although it can happen. However, a majority of diabetics do take insulin, and hypoglycemia is quite common in this population. In fact, 80% of people with type 1 diabetes and over half with type 2 diabetes will experience hypoglycemia at least once per month.
There are additional risk factors for hypoglycemia:
- Aged 65 years or older
- Previous case(s) of low blood sugar
- Other health conditions, including kidney disease, heart disease, or cognitive impairment
What are the symptoms of hypoglycemia?
There are a wide variety of hypoglycemia symptoms; and repeated hypoglycemia can cause an individual to lose sensitivity to the signs of hypoglycemia, making serious hypoglycemia more likely. Additionally, some common diabetes-related conditions (including cardiac and stroke) can have similar symptoms, which can lead to hypoglycemia going unnoticed in the hospital.
A good understanding of hypoglycemia symptoms can help make sure a mild episode never turns severe. Symptoms are usually grouped into two categories:
Adrenergic symptoms: resulting from rapidly falling blood sugar. These adrenergic symptoms can function as an early warning system when they occur before neuroglycopenic symptoms.
Symptoms include:
- Anxiety
- Irritability
- Dizziness
- Sweatiness
- Pale skin
- Rapid heartbeat
- Headache
- Shakiness/tremors
- Hunger
Neuroglycopenic symptoms: resulting from low systemic blood sugar impacting the central nervous system.
- Cognitive impairments
- Behavioral changes
- Psychomotor abnormalities
- Seizures (very low blood sugar levels)
- Coma (very low blood sugar levels)
The following table depicts the sequence of responses that occur as blood glucose levels fall. In healthy individuals, physiological defenses work to abort developing hypoglycemia. In people with type 1 diabetes and advanced type 2 diabetes, however, these defenses against hypoglycemia are typically compromised. Thus, it is critical to raise “hypoglycemia awareness” — including recognition of the early symptoms (cited above) and the preventative strategies we’re about to discuss.
Table: Physiologic responses to decreasing plasma glucose concentrations
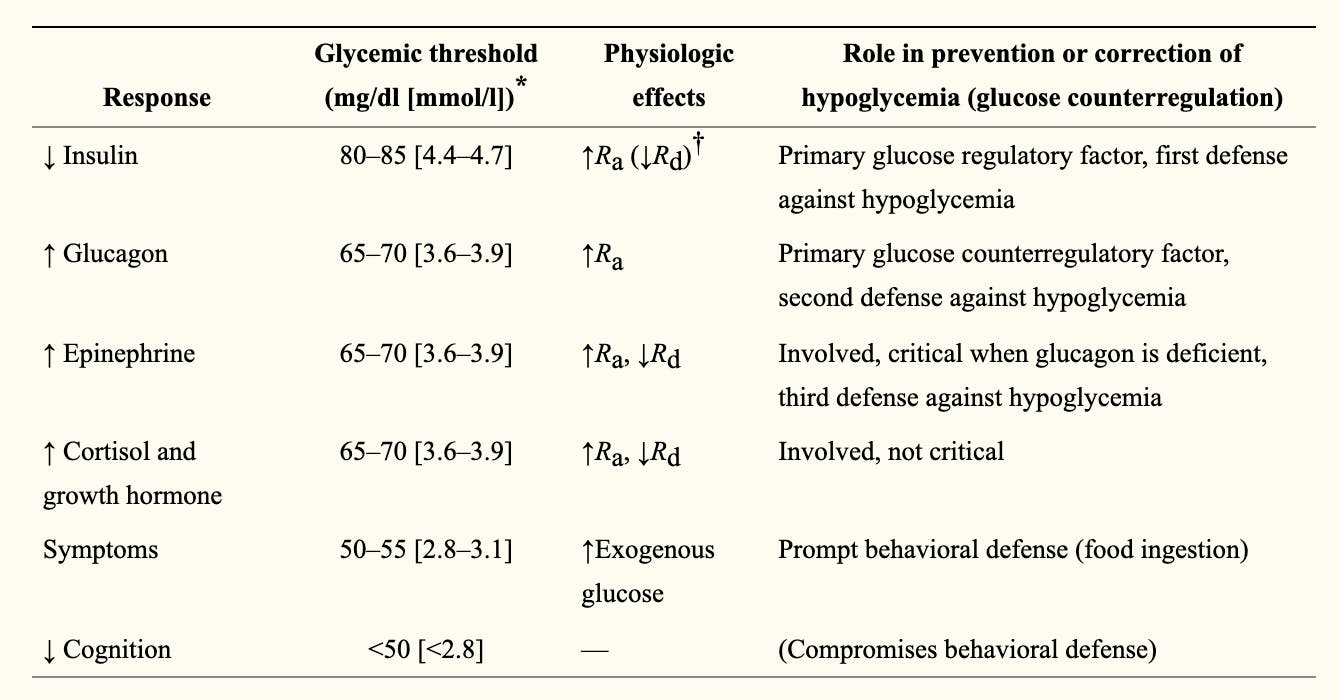
Source: NCBI
Because symptoms of hypoglycemia are varied and often similar to symptoms of other conditions, the “Whipple’s triad” must be met to confirm a case of hypoglycemia:
1) symptoms of hypoglycemia,
2) a low blood sugar measurement, and
3) relief of symptoms after blood sugar levels are restored to normal.
How to prevent hypoglycemia
There is no evidence that repeated hypoglycemia causes long-term neurological impairments in adults with diabetes, but we still don’t know whether this is also true for children or elderly individuals. However, repeated hypoglycemia does cause the body to lose its ability to detect and react to hypoglycemia (this is discussed more below).
Controlling blood sugar levels can not only ensure your body doesn’t lose its detection ability, but it can also help minimize the risk for common diabetes comorbidities such as retinal disease, loss of kidney function, and nerve damage.
One of the biggest ways to avoid hypoglycemia is to use the correct dosage of glucose-altering medications and to eat the right amount of carbohydrates. Both practices are specific to the individual, can change over time, and should be carefully monitored and adjusted by the patient’s doctor.
Additionally, there are other important things to consider for preventing hypoglycemia:
- Because alcohol consumption can lower your blood sugar level, it is advisable to only consume alcohol in moderation or not at all. If you do consume alcohol, make sure you also eat food (which increases blood sugar) while drinking.
- Exercise increases the amount of sugar needed by your muscles, and therefore lowers blood sugar levels. Be sure to eat/drink simple carbohydrates before and after exercise to prevent hypoglycemia. Your doctor might also suggest adjusting medications.
- Meals low in carbohydrates do not raise blood sugar levels very much. Blood sugar levels should be carefully monitored if carbohydrate intake is low so that falling blood sugar levels can be quickly addressed.
- Insulin sensitivity increases when a person loses weight, if their fitness has improved, and if they’ve been able to control blood sugar levels consistently. In any of these circumstances, adjusting blood sugar-altering medications, such as insulin, might be necessary to avoid hypoglycemia.
- If a person with diabetes is admitted to the hospital for any reason, extra special care must be taken to monitor blood sugar levels since symptoms of hypoglycemia mimic those of other conditions.
It is also critical to avoid the development of hypoglycemia-associated autonomic failure (HAAF). HAAF occurs when multiple episodes of hypoglycemia cause a defect in the body’s natural response to countering hypoglycemia while dulling the neurogenic response to hypoglycemia (i.e., obvious symptoms don’t occur). This leads to a vicious cycle of hypoglycemia, unawareness of the hypoglycemia, hypoglycemia again… which can ultimately lead to severe hypoglycemia. Fortunately, this condition can be reversed if hypoglycemia is prevented completely for a few weeks.
Because HAAF can also occur after exercise or sleep, care should be taken to carefully monitor blood sugar levels for up to 15-24 hours after exercising as well as upon waking up. If necessary, carbohydrate consumption and/or medication can be adjusted appropriately to prevent or address falling blood sugar levels.
Key takeaways
Hypoglycemia is a way of life for many people with diabetes, especially those taking insulin or other medications that alter blood glucose levels. Fortunately, severe hypoglycemia is rare, and can be avoided or quickly treated with a combination of blood glucose monitoring, appropriate food and beverage consumption, and medicine dosage. Taking care when consuming alcohol, exercising, or losing weight can also ensure blood sugar levels don’t go too low. To get a handle on your blood sugar levels and avoid hypoglycemia, talk to your doctor to determine your personal healthy blood sugar level, establish a blood sugar checking routine, and select the best lifestyle and medicine interventions. With the right tools, a healthy life is possible for those with diabetes.