The Link Between Blood Sugar and Diabetes
Here’s what happens when your blood sugar spikes—and what it could mean for your long-term health.
January 26, 2021

Article Summary: Diabetes & Blood Sugar
Stop us if this sounds familiar: You grab yourself an ice cold soda (nope, not the diet kind) and as you slurp it down—wham!—you feel a jolt of energy. Ah, the buzz of a sugar high. We’ve all been there. Whether we’re searching for a quick pick-me-up or feel ambushed by the rush, the effects of sugar on our bodies are definitely noticeable. But have you ever wondered what’s really going on, biologically, to cause that sudden boost of energy? Understanding the biology of blood sugar (aka glucose) makes the link between the food we eat and our risk of diabetes crystal clear. And knowledge is power, when it comes to protecting this key element of metabolic health.
Odds are, if you’ve found out that you have prediabetes or diabetes, you’ve heard a lot about blood sugar and why you need to keep it in check to stop these conditions from worsening. What’s the connection exactly? Well, when sugar enters your bloodstream, your pancreas creates insulin which is responsible for getting that sugar out of the blood and into your cells so it can be used for energy to keep your vital organs working properly. That is, if you’re eating a balanced amount of sugar to keep your body humming along. Too much sugar, however, can cause serious problems and affect your body’s ability to produce insulin and get sugar out of the blood.
When you have diabetes, your pancreas either can’t make enough insulin or your body no longer uses the insulin it does produce properly. This means that more sugar stays in your bloodstream because less of it gets offloaded into your cells. The result: chronically high blood sugar levels, and a higher risk of chronic diseases.
How Your Body Handles Sugar
Knowing how your body responds to sugar is one of the keys to understanding the connection between blood sugar, overall health, and diabetes. It’ll help if we start with a quick high school biology refresher on what happens as the food you eat turns into fuel for your body:
- During digestion, the carbs you consume are broken down into sugar (known as glucose) that is released into your bloodstream.
- As a result, your blood sugar levels will rise, which triggers your pancreas to get to work producing insulin, a hormone needed to move that sugar out of your blood and into your cells so it can be converted into energy.
- Insulin unlocks cells so they absorb glucose, powering all of your body’s systems and functions.
- Any extra glucose that your body doesn’t need for energy at that moment is stored in the liver.
- When insulin levels drop, your body taps the liver’s backup supply to keep energy levels nice and stable.
And so it goes when your body is fueled well and working as it should. Blood sugar levels rise and fall gently, with no wild swings up and down. What happens when unhealthy eating and other lifestyle choices bring on sugar highs and crashes? Your body is stressed. “On occasion this can be fine,” says Maziyar Saberi, PhD, a systems physiologist and Chief Scientific Officer at January AI. “Our bodies, under healthy conditions, can maintain blood glucose in a normal range, even when we sometimes don’t eat well. But when glucose is routinely on a massive roller coaster, systems that regulate blood glucose begin to malfunction and eventually deteriorate.” As a result, you may experience exhaustion, hunger and cravings, moodiness, brain fog, weight gain, and more. If and when diabetes develops, it means the process of metabolizing blood sugar has gone completely haywire in your body, and management becomes key not just to feeling good, but to your long term health.
What is Diabetes?
Diabetes occurs when your pancreas either can’t make enough insulin, or your body no longer uses the insulin it does produce effectively. This means that more sugar stays in your bloodstream because less of it gets offloaded into your cells. The result: chronically high blood sugar levels. If untreated, this can come with serious consequences, including the risk of developing heart disease (as high blood sugar can damage arteries), kidney failure, nerve damage, and even blindness.
There are two types of diabetes. Type 1 is rarer and typically develops early in life, due to either genetics or an autoimmune response. We’re going to focus on Type 2, which is a much more common but preventable form of the disease that most often develops in adulthood as a result of a host of factors, including eating habits, lifestyle, and genetics. And it affects a lot of us: The American Diabetes Association estimates that roughly 34 million American adults have diabetes—and a whopping 7 million of them have no idea because their condition has gone undiagnosed.
What is Prediabetes?
Prediabetes is the stage before full-blown type 2 diabetes in which your blood sugar levels have shifted past the normal range but aren’t so high that they’ve reached the diabetic zone. According to the American Diabetes Association, a staggering 88 million Americans over the age 18 have prediabetes. Most people have no idea, unless they’ve received something called an A1C test to measure their blood sugar (it requires a simple blood draw). While those with prediabetes may never develop the full-blown disease, they are at increased risk unless they make lifestyle changes, which includes eating a healthier diet and exercising regularly. “The good news,” says Saberi, “is that at this point, type 2 diabetes is often preventable and under our control. Changes in nutrition and physical activity are by far the most effective approaches to preventing diabetes and related health issues. But the secret is identifying what works best for each individual. There is no one-size-fits-all approach.”
The A1C Test
The A1C test measures your average blood sugar levels over the last two to three months. Think of it as a picture of your current health and how well your body is regulating its glucose.
- Normal: Below 5.7%
- Prediabetes: 5.7% - 6.4%
- Diabetes: 6.5% or above
Depending on where your results fall, your doctor may suggest making changes to your lifestyle to bring your number down. But keep in mind: Once you’ve hit above 6.5%, you’ll be living with diabetes for good. Yes, you can get your numbers back down, but because you’ve crossed that threshold, you’re at increased risk of climbing back into that range. “That diagnosis can be frightening, but diabetes doesn't have to be permanent,” says Saberi. “If diagnosed in the early stages, it can be reversed with simple changes. What’s more complex, and sometimes frustrating, is identifying what you need to change or modify.” Your doctor will help you determine the best way to monitor and test your blood sugar levels to keep it in a safe zone throughout any given day. And you have the power to maintain healthy levels with every choice you make around food and activity, as well as sleep, and stress levels.
When Blood Sugar Spikes
Whether you’ve been tested for diabetes or not, you may have started to notice how your body responds to certain foods. Different foods will spike blood sugar levels to different degrees, depending on a variety of factors. Sure, it matters how much carbohydrate (particularly added sugar) your food contains, but the amount of fiber, protein counts, too. The goal is to eat well so your blood sugar levels stay stable, with small rises and dips instead of big, sharp swings in either direction. We should all follow general nutritional guidelines, but also realize that every person’s sugar response is unique. For example, you might struggle to manage blood sugar after eating bananas, while your friend who has a similar health profile to yours can eat them with no problem. It’s vital to be in tune with your body, because until levels get past a certain threshold, it’s easy to be affected by high blood sugar but not recognize it.
Once diabetes develops, the symptoms are much harder to miss. A glucose “rush” might come with:
- Frequent urination
- Chronic Fatigue
- Increased thirst
- Blurry vision
On the flip side, when your blood sugar levels bottom out, you’ll feel that dreaded crash. When this happens and your blood sugar levels are too low, you may notice that you experience:
- Dizziness
- Irritability
- Sweating
- Lack of coordination
Bottom line
Everyone is different. The best way to understand the effect of sugar on your body is to pay attention to how you feel. One easy way to start is to keep track of how your body feels after you eat certain foods—do you notice an energy spike, then crash? Do you feel fueled and focused, but not buzzed or moody? Take note of how your body responds to your daily diet and see this as your baseline. You can begin to make changes from there. Gaining an understanding of how your body responds is the first step in making sure you’re nourishing it well.
FAQs
Does diabetes affect blood sugar levels?
Yes! Diabetes occurs when your blood sugar levels rise above a certain threshold. It’s marked by having an A1C blood test at 6.5 percent or above. This occurs when your pancreas is no longer able to make enough insulin to get sugar out of the blood and into your cells or when your body has plenty of insulin to do the job but your cells are unresponsive. The result is that more sugar stays in your blood than is healthy.
What are normal blood sugar levels for someone with diabetes?
Blood sugar levels naturally fluctuate in all of us, depending on what we’ve eaten, the time of day, if we’ve just exercised, how stressed we are, and more. Rises and falls of blood sugar are perfectly normal throughout the day. When these changes are subtle, you won’t notice them much because your system is keeping your energy supply mostly stable. However, when blood sugar swings go way up and then way down, you may experience bursts of energy, followed by crashes, and a host of other symptoms
For people with diabetes, there are certain ranges you want to stay in so you know you’re managing the condition well and preventing major damage in your body:
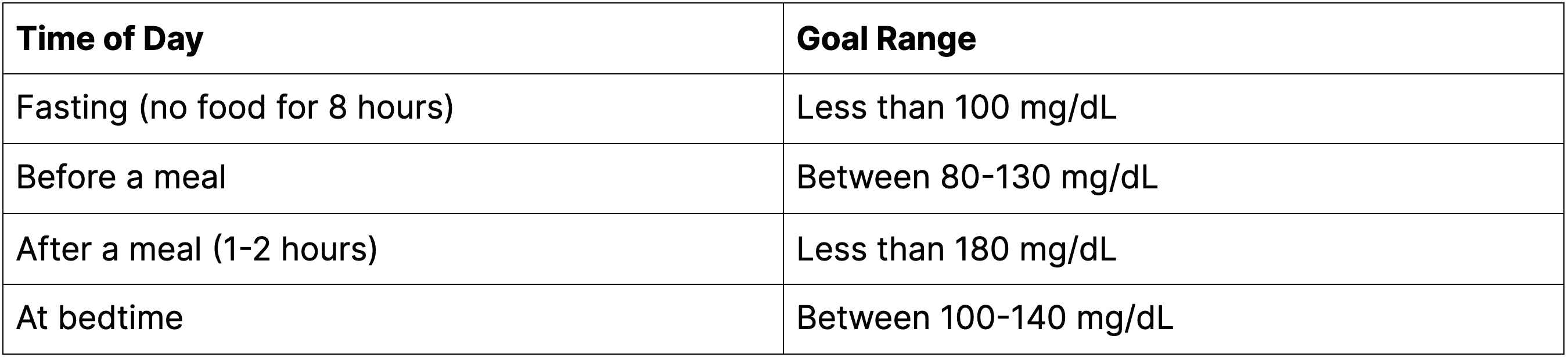
Source: American Diabetes Association
Keep in mind: These are just general guidelines. If you have diabetes, speak with your healthcare professional about what numbers you should strive for throughout the day based on your unique situation.
Why would a type 2 diabetes blood sugar level be high in the morning but way lower throughout the day?
There are several reasons you may wake with a blood sugar level that’s higher than you’ll see throughout the day. For example, if you take medication, it could be that you didn’t have enough the night before or that you ate a high-carb snack prior to bed which sent sugar into your bloodstream that remained through the night.
There’s also something called the “dawn phenomenon” that can cause an early morning jump in blood sugar, during the hours of 3 am and 8 am. This occurs when your body starts producing more glucose so you have the energy you need to get you up and going for another day. Additionally, if you take medication, it could be wearing off, creating a perfect storm for an AM spike. Once you understand what’s causing the morning spike, you can work with your doctor to tweak your morning and evening routines so things stay more stable.