What is “Time in Range” and Why is it Important for Metabolic Health?
If you’re tracking your blood sugar, these are the numbers you need to know.
January 26, 2021

Article Summary: Your “Time in Range” Snapshot
There are a host of reasons you may want to dig deeper into your blood sugar (aka glucose) control. Maybe your doctor just gave you an A1C test and the results put you in the prediabetes category. You may already have full-blown diabetes, or just a family history of the disease that has you worried and ready to change your lifestyle to protect yourself. You may have perfectly normal numbers and want to make sure it stays that way. In all three cases it helps to have benchmarks to understand the distance between where your glucose levels are now and where you need them to be.
Your doctor can do a variety of blood tests to capture your glucose levels under different circumstances (following a long break from eating, for example.) “Time in range” is measured using a continuous glucose monitor (CGM). This small device attaches painlessly to your arm and monitors your blood sugar levels all day and night, with no needles or waiting for test results. As you eat, digest, and move, you’ll watch your glucose rise and fall, see when it spikes high or dips low, and when it holds relatively steady. Time in Range (TIR) is the amount of time your body spends in its target healthy zone for glucose levels. If you’re on the diabetes spectrum, this is when things are most stable for you, and you’re on track to avoid complications, like heart disease and kidney damage. According to 2019 guidelines published in the American Diabetes Association’s journal Diabetes Care, TIR is defined as the time spent in a target range between 70 and 180 mg/dL for those with diabetes. Even if you don’t have diabetes or are only at the prediabetes stage, there are overall ranges that are good for you to know so you can evaluate your metabolic health. For people without diabetes, or those trying to keep their diabetes in tight control, 70 to 140 mg/dL is the generally accepted target range.
Whatever your current health status, using a CGM to monitor time in range can give you a sense of how your body responds to different kinds of foods and activities, so you know exactly what changes to make for better glucose control.
What range should my blood sugar levels be?
If you’re not using a CGM, your doctor may perform different kinds of blood tests to measure your blood sugar. A random glucose test is taken at any time, no fasting or preparation needed. A fasting test, on the other hand, requires at least eight hours without food (and is usually taken first thing in the morning to make it easier on you). A post-prandial test is one taken two hours after a meal. It can help determine your blood sugar as it relates to food, which may provide insights into your body’s current ability to regulate glucose.
Why so many different tests? Doctors like to see how well your body is controlling glucose under the various conditions you cycle through in any given day. Fasting is a great first-thing-in-the-morning baseline and is the one most often used to diagnose diabetes. The table below will give you an idea of the ranges used to determine if you’re on the diabetes spectrum, and where along that spectrum you might be.
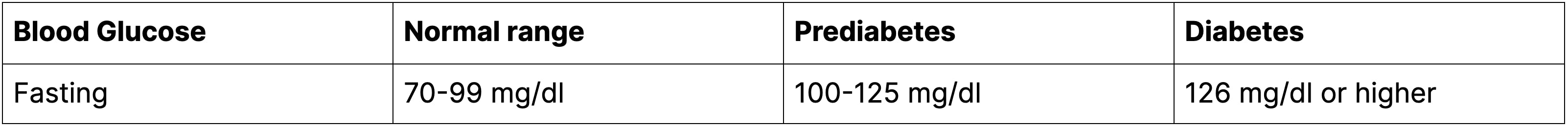
Source: American Diabetes Association
What Are the Time in Range Targets for Someone With and Without Diabetes?
Glucose levels fluctuate throughout the day, so it’s normal to see a curve with little peaks and valleys. But the gold standard is 100% TIR (which translates to all 24 hours), with the range defined differently for people with and without diabetes. Those without, who are aiming for optimal metabolic health, would try to stay within a range of 70 to 140 mg/dl for as much of the day as possible. People with diabetes might give themselves a bit more wiggle room, aiming for a high percentage of the day in a range of 70 to 180 mg/dl.
Keep in mind: These are just targets, so they aren’t personalized to your specific situation. You should always consult with a medical professional about the right TIR goals for you, which can shift for a variety of reasons, including if you’re pregnant, older, or at high-risk for complications.
Why is Time in Range Important?
We’ve talked a lot about TIR, but the A1C test is the current standard for tracking prediabetes and diabetes because it tells you the average of your glucose levels over the course of the last two to three months. The results provide a big-picture view of how your body is handling glucose, and can’t be thrown off by, say, the pizza you had last night or the half-cookie you just scarfed. It’s the measure most doctors use to track your progress and diabetes management over time. An A1C level between 5.7% and 6.4% is classified as prediabetes. Anything at 6.5% or above indicates diabetes.
Of course any test that takes an average of your results over a long period of time misses the spikes and dips you may be experiencing on a daily basis, which can be problematic. “For example, three people could all have an A1C level of 7, but one is spiking up and down repeatedly throughout the day, another might hit highs but rarely go low, and another might never venture out of the healthy zone,” says Maziyar Saberi, PhD, systems physiologist and January AI Chief Scientific Officer. “All might have an average of 154 mg/dL, for an A1 of 7 over time, but the effect on their bodies is very different. Constant and excessive spikes will eventually take a toll on the metabolic system and it will begin to deteriorate. This could happen years before disease shows up, and without the individual knowing.”
In addition, the A1C test has been shown to fall short at detecting hypoglycemia, in which your blood sugar levels are lower than normal (below 70 mg/dL). This can be dangerous: Severe hypoglycemia can lead to seizures or cause you to lose consciousness. In fact, a 2018 study in the journal Clinical Diabetes found that 92 percent of hospitalizations related to hypoglycemia were among those with type 2 diabetes.
All this explains why tracking your TIR with a CGM can be so valuable. You’ll be able to see throughout the day if your levels are spiking and dipping (which can happen), but more importantly, how long you’re staying out of your optimal range and when those excursions occur. If you don’t have diabetes, this can help you make small but meaningful lifestyle tweaks—fewer carbs at dinner or more exercise after lunch, for example—to keep your levels more stable. If you do have diabetes, this type of data can help your care team modify your approach so you spend more time in a healthy glucose range and less time below or above it.
Doctors still recommend A1C testing in conjunction with TIR tracking for a well-rounded approach to your care.
What Should My Time in Range Goal Be?
You may feel gung-ho about staying in your TIR target zone most of the time—and that’s great. For people who haven’t been diagnosed with diabetes or prediabetes, a CGM can help you get there, and in record time. You’ll see the foods that cause glucose jumps, the ones that prevent them, and how activity can come to the rescue and level a potential spike.
For those on the diabetes spectrum, 100% TIR may not be realistic, at least at first. The researchers who set the TIR guidelines recommend focusing on reducing your Time Below Range (TBR) time initially. This means reducing your chances of experiencing hypoglycemia. Start by asking yourself a few questions: When do your numbers dip below the bottom of your range? How long are you below range? Does it change based on when and what you eat? The answers let you start to see how your lifestyle may contribute to more time in TBR and what changes you may want to make to reduce the frequency of those dips. For example, you might aim to limit your TBR to less than one hour per day. And you might switch up how many carbs you eat or when you exercise to achieve that. “CGMs are a game changer here because they provide direct glucose levels without the need for typical symptoms that accompany hypoglycemia,” says Saberi. “And hypoglycemia is far more dangerous than hyperglycemia, especially for insulin users.”
Bottom line: Using a CGM will help you look for patterns and discover the habit shifts and new routines that make sense for your health and lifestyle. The idea is to make small, realistic changes that you can stick with so move you closer to the ideal TIR targets for your health.